2.2.3.16 Special Information's on the Anesthetic Technique by Minimally Invasive Total Knee Arthroplasty (MIS TKA)
Details information's on the anesthetic procedure for your Minimally Invasive Total Knee Arthroplasty will be informed by our colleges Department of Anesthesia in the Spital Oberengadin. These information's will be handled out with a “questionnaire and patients information sheet” and you will be informed personally within a separate meeting with one of the staff-members of the department of anesthesia.
Für weitere Informationen über den sog. "Fragen- und Patientenaufklärungsbogen:
Auf Deutsch: Bitte hier drücken
In Italiano: Per favore puntare il pulsante qui
In English: Please click here
Further information about the Department of Anesthesia in the Spital Oberengadin, under direction of Dr. Mark Brouwer and with the collaboration of Dr. Floris Tichler and Dr. Michael Stephan, are available www.spital-oberengadin.ch/Index.
The following text therefore mainly contains information's on the anesthetic technique by a Minimally Invasive Total Knee Arthroplasty (MIS TKA).
Anesthesia in MIS TKA should provide adequate pain relief and muscle relaxation during the procedure and minimize post-operative pain. For post-operative pain control, our patients receive first a one-off sciatic nerve block (SB), and then a continuous femoral nerve block (FB). Regional techniques are performed on conscious, only slightly premedicated patients (10 µg of sufentanyl (Sufenta, Janssen-Cilag AG, CH-6341 Baar, Switzerland) intravenously shortly before starting the procedure), using a neurostimulation device (Stimuplex HNS 11, Braun Melsungen AG, D-34212 Melsungen, Germany) and stimulating needles.
The single-shot sciatic nerve block (SB):
Anatomy of the Sciatic Nerve:
The sciatic nerve is the largest nerve in the body, measuring about 2 centimetres in thickness in its proximal portion. At this location, it is actually composed of the sciatic nerve and the posterior cutaneous nerve of the thigh. This "double nerve" contains contributions from the lumbar nerve roots 4 and 5 and the sacral nerve roots 1, 2 and 3.
Technique:
The single-shot sciatic nerve block (SB) is performed in the classical Labat approach with the patient in the lateral position, exposing the affected side (Fig. 1). The needle (Polymedic® UPC G23, 150 mm) is advanced towards the sciatic nerve until foot movements can be elicited at a threshold of 0.4 mA, 0.1 msec. A total of 15-20 mL ropivacain 0.75% (Naropin®, Astra Zeneca AG, CH-6301 Zug, Switzerland) is administered. This dose usually provides satisfactory analgesia for over 24 hours. Alternatively, especially in immobile patients, the anterior or lateral approach for IB (modified according to Meier) can be used.

Figure 1. The single sciatic nerve block is done following the technique of Labat: The patient is first placed in the lateral position with the side to be blocked up. While the lower leg is kept straight, the thigh is flexed at the knee so that the ankle is brought over the knee of the other leg. The important bony landmarks to block the sciatic nerve via the two posterior approaches are the greater trochanter (A), posterior superior iliac spine (B) and the ischial tuberosity (C). A line is drawn between the greater trochanter (A) and the posterior superior iliac spine (B). The line lies approximately over the upper border of the piriformis muscle. From the midpoint of this line (D), at right angles to it, a second line passing over the buttock is drawn. The point of injection is 3 - 5 centimetres along this perpendicular line. It can be more precisely identified by drawing a third line between the greater trochanter and sacral hiatus, the point of injection being where this third line intersects with the second, perpendicular line.
The continuous femoral nerve block (FB):
Anatomy of the femoral nerve:
The femoral nerve receives contributions from the second, third and fourth lumbar nerves. It is derived from the lumbar plexus and in fact lies within the same fascial envelope as the lumbar plexus. This important fact may be utilised to block most of the nerves originating in the lumbar plexus with a single injection distally, as local anaesthetic can be made to spread proximally within this plane.
Technique:
The femoral nerve block (FB) is done back in the supine position (Fig. 2). The catheter is placed using the classic paravascular Winnie approach. The needle (Borgeat C 70T, Polymedic®) is advanced until contractions of the quadriceps femoris muscle, at a threshold of 0,4 mA, 0.1 msec. indicate accurate positioning of the needle tip in the immediate proximity of the femoral nerve. After negative aspiration, 10 mL of Lidocain 1% (Xylocain®, Sintetica SA, CH 6850 Mendrisio, Switzerland) are injected. The needle is removed and the catheter advanced 5 to 10 cm through the plastic cannula. After subcutaneous tunneling (5 cm) and application of a bacterial filter, another 10 mL of Lidocain 1% are injected.
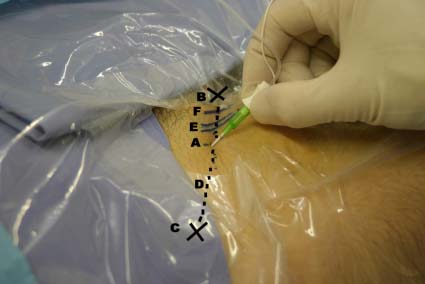
Figure 2. The femoral nerve block (FB) is performed with the patient supine following the technique of Winnie. The important bony landmarks for blocking the femoral nerve (A) are the pubic tubercle (B), the anterior superior iliac spine (C), the inguinal ligament (D), and the lateral border of the femoral artery (E), and the femoral vein (F) at the inguinal crease. For the femoral nerve (A), the point of injection lies just below (distal to) the inguinal ligament (D). Palpate both the anterior superior iliac spine (C) and the pubic tubercle (B). The line between these two overlies the inguinal ligament (D). It is often helpful to draw lines on the skin. The femoral artery (E) should lie at the midpoint of the inguinal ligament and it is necessary to locate this by palpating the pulse at this point. The site for injection is 1 cm lateral to lateral edge of the pulse of the femoral artery and 1 - 2 cm below (distal to) the line of the inguinal ligament.
Because of the inconsistent blockade of the obturator nerve with the previously described blocks, the operation is performed with an additional lumbar spinal anaesthesia (Reganesth Pencil Point G27, hyperbaric Bupivacaine 0.5% 2.5-3 ml, B. Braun Medical AG, CH-6204 Sempach, Switzerland), or general anesthesia (i.e. Propofol (Disoprivan®, Fresenius Kabi AG, CH-6371 Stans, Switzerland), Remifentanil). Immediately post-operatively, the femoral catheter is connected to a patient-controlled analgesia pump (PCA), delivering ropivacaine 0.2% (Naropin®), usually set at a basic rate of 6 ml/h, with a 4 mL bolus function and a 30 minutes lock out time. The setting is then adjusted according to the individual pain scores and symptoms (particularly motor blockade) during daily ward rounds. The femoral catheter is usually left in place for 48 – 72 hours, depending on the patient individual requirement.
If you would like to download these information's as a PDF file, please click here
Gonarthrose:
Zurück auf dem Index: Bitte hier klicken
